CENTRAL SEROUS CHORIORETINOPATHY
Definition
• Central serous chorioretinopathy (CSCR) is an idiopathic disorder characterized by a localized serous detachment of the neurosensory retina in the macular region. secondary to leakage from the choriocapillaris through focal, or less commonly diffuse, hyperpermeable RPE defects.• CSCR typically affects one eye of a young or middle-aged Caucasian man; women with CSCR tend to be older.
• Imperfectly defined additional risk factors include psychological stress, type A personality, steroid administration, Cushing syndrome, systemic lupus erythematosus and pregnancy.
Etiopathogenesis
Risk factors include:
• Age & sex: The disease affects typically young adult (20-50 years), males more than females. (6:1)• Personality: Type A personality individuals are more prone.
• Emotional stress
• Steroid intake
• Hypertension
• Pregnancy (usually 3rd trimester)
• Cushing’s disease
Pathogenesis
- It is not known exactly.
- It is now believed that an increase in choroidal hyperpermeability causes a breach in the outer blood retinal barrier (a small opening or blow out of RPE).
- Leakage of fluid across this area results in development of localized serous detachment of neurosensory retina.
- What triggers the choroidal hyperpermeability is poorly understood.
- It is being suggested that an imbalance between the sympathetic parasympathetic drive that maintains autoregulation within the choroidal vasculature may be defective in patients with CSR.
Clinical features
Symptoms: Patient presents with a sudden onset of painless loss of vision (6/9-6/24).
Presentation is with unilateral metamorphopsia that may be associated with relative positive scotoma, micropsia, mild dyschromatopsia and decreased contrast sensitivity.
VA is usually reduced to 6/9–6/18, but often correctable to 6/6 with a weak convex lens, because elevation of the sensory retina gives rise to an acquired hypermetropia.
Signs
- Mild elevation of macular area, demarcated by a circular ring-reflex.
- Foveal reflex is absent or distorted.
- A round or oval detachment of the sensory retina is present at the macula.
- The subretinal fluid may be clear (particularly in early lesions), turbid or fibrinous, and precipitates may be present on the posterior retinal surface.
- Small yello-grey elevations may be seen due to RPE detachment.
- One or more abnormal depigmented RPE foci (sometimes small PEDs) of variable size may be visible within the neurosensory detachment.
- Small patches of RPE atrophy and hyperplasia elsewhere in the posterior pole may indicate the site of previous lesions.
- Multifocal pigmentary changes suggest chronicity.
- The optic disc should be examined to exclude a congenital pit.
Investigations
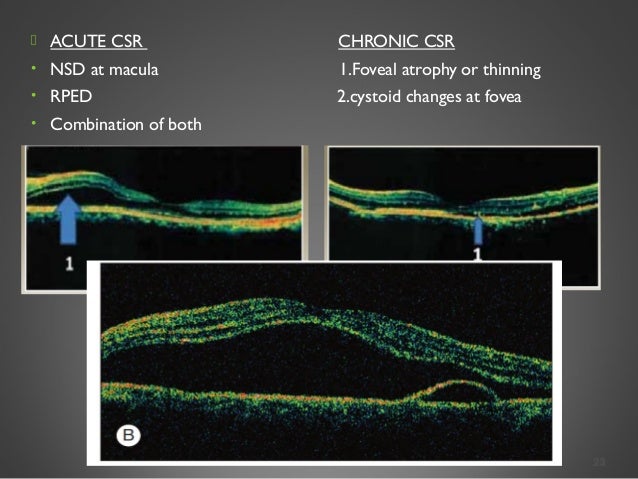
1. Amsler grid confirms metamorphopsia corresponding to the neurosensory detachment.FFA helps in confirming the diagnosis. Two patterns of progressive leakage and pooling from one or more points seen are:
• 'Smokestack’ pattern manifests as an early hyperfluorescent spot that progresses to form a vertical column by the late venous phase, followed by diffusion throughout the detached area. It consists of small hyperfluorescent spot which ascends vertically like a smoke-stack & gradually spreads laterally to take a mushroom or umbrella configuration.
• ‘Ink blot’ pattern (most common) shows an early hyperfluorescent spot that gradually enlarges.
• An underlying PED may be demonstrated.
• Multiple leakage points or diffuse leakage can be evident, particularly in chronic or recurrent disease.
4. ICGA. The early phase may show dilated or compromised choroidal vessels at the posterior pole. The mid-stage shows areas of hyperfluorescence due to choroidal hyperpermeability.
Course
CSR is usually self limiting but often recurrent. Three patterns are known:normal vision in more than 80% but recurrences occur in up to 50% of cases.
• Short clinical course is characterized by spontaneous resolution within 3-6 months with near normal visual recovery. Recurrences are known in 30-50% of all the cases.
2. Chronic course lasting more than 12 months constitutes a minority and typically affects older patients.
• Prolonged detachment is associated with gradual photoreceptor and RPE degeneration with resultant visual impairment.
• Multiple recurrent attacks may also give a similar clinical picture.
• FA shows granular hyperfluorescence with one or more leaks.
• CMO, CNV or RPE tears may develop in a minority of cases.
Differential diagnosis
• Optic pit
• Idiopathic polypoidal choroidal vasculopathy
• Macular hole with serous detachment
• Choroidal tumors
• Pigment epithelial defect
Management:
1. Observation is appropriate in most cases. Since CSR undergoes spontaneous resolution in 80-90% cases. Visual acuity returns to normal or near normal within 3-6 months.2. Discontinue any corticosteroid treatment if possible, particularly in chronic, recurrent or severe cases.
4. Laser photocoagulation to the RPE leak speeds resolution but does not influence the final visual outcome or recurrence rate.
Indications:
• Long standing cases (more than 6 months)
• Patients having recurrent CSR with visual loss.
• Patients having permanent loss of vision in the other eye due to this condition.
Contraindication:
5. PDT may be considered in subfoveal leaks or chronic disease.
(severe disease Not amneble to conventional laser treatment) Only 30% of the dose of verteporfin used for CNV, in conjunction with 50% light intensity is used by some authorities as first-line treatment.
6 Intravitreal anti-VEGF agents can be considered if CNV develops.



No comments:
Post a Comment