XEROPHTHALMIA
Xerophthalmia refers to the spectrum of ocular disease caused by lack of vitamin A, and is a late manifestation of severe deficiency.
They term xerophthalmia is now reserved (by a joint WHO and USAID Committee, 1976) to cover all the ocular manifestations of vitamin A deficiency, including not only the structural changes affecting the conjunctiva, cornea and occasionally retina, but also the biophysical disorders of retinal rods and cones functions.
Etiopathogenesis
Vitamin A is essential for the maintenance of the body's epithelial surfaces, for immune function and for the synthesis of retinal photoreceptor proteins.
It occurs either due to dietary deficiency of vitamin A or its defective absorption from the gut.
Lack of vitamin A in the diet may be caused by malnutrition, malabsorption, chronic alcoholism or by highly selective dieting.
It has long been recognised that vitamin A deficiency does not occur as an isolated problem but is almost invariably accompanied by protein-energy malnutrition (PEM) and infections.
The risk in infants is increased if their mothers are malnourished and by coexisting diarrhoea or measles.
WHO classification (1982)
The new xerophthalmia classification (modification of original 1976 classification) is as follows:
XN Night blindness
X1A Conjunctival xerosis
X1B Bitot’s spots
X2 Corneal xerosis
X3A Corneal ulceration/keratomalacia affecting less than one-third corneal surface
X3B Corneal ulceration/keratomalacia affecting more than one-third corneal surface.
XS Corneal scar due to xerophthalmia
XF Xerophthalmic fundus.
Clinical features
1. XN (night blindness).
Vit A (retinol) deficiency affects rhodopsin production, impair rod functions – leads to night blindness (nyctalopia)
It is the earliest symptom of xerophthalmia in children.
It has to be elicited by taking detailed history from the guardian or relative.
Response to Vit A – rapidly, within 24 to 48 hours of therapy
2. XlA (conjunetival xerosis).
It consists of one or more patches of dryness, lusterless, nonwettable conjunctiva,
(dryness, lack of wettability, thickening, wrinkling, and pigmentation in temporal interpalpebral conjunctiva)
(soft sign of VAD diagnosis but reliable when extend to inferior palpebral conjunctival region)
Which has been well described as 'emerging like sand banks at receding tide' when the child ceases to cry.
These patches almost always involve the inter-palpebral area of the temporal quadrants and often the nasal quadrants as well.
In more advanced cases, the entire bulbar conjunctiva may be affected.
Typical xerosis may be associated with conjunctival thickening, wrinkling and pigmentation.
(Xerosis is characterized by dryness of the conjunctiva in the interpalpebral zone with loss of goblet cells, squamous metaplasia and keratinization.)
 |
| Figure 1. Conjunctival xerosis. Note the slight wrinkling of the temporal conjunctiva |
3. XlB (Bitot's spots).
It is an extension of the xerotic process seen in stage X1A.
The Bitot’s spot is a raised, silvery white, foamy, triangular patch of keratinised epithelium, situated on the bulbar conjunctiva in the inter- palpebral area. It is usually bilateral and temporal, and less frequently nasal.
Bitot spots are light-grey triangular patches with foamy surface in temporal or nasal interpalpebral bulbar conjunctiva zone, frequently
bilateral - represents area of conjunctival keratinized epithelium, acanthotic thickening and loss of goblet cells –(sings of xerosis), Foamy appearance is caused by Corynebacterium xerosis with combination of mucus and keratin)
Response to Vit A – resolve within 2 to 5 days of therapy, most disappear in 2 weeks
 |
| Figure 2. Bitot's spots at the temporal limbusAdd caption |
4. X2 (corneal xerosis).
Involved cornea lacks lustre with dryness. (Lustreless appearance due to secondary xerosis)
The earliest change in the cornea is punctate keratopathy which begins in the lower nasal quadrant –progressing to involve entire corneal surface.
(Bilateral punctate corneal epithelial erosions in the inter-palpebral zone in early lesions – progress to epithelial defects- Keratinized plaques )
Followed by haziness (corneal stroma edematous) and/or granular pebbly dryness.
Response to Vit A – respond within 2 to 5 days of therapy, normal appearance in 1-2 weeks
 |
| Figure 3. Corneal xerosis |
5. X3A and X3B (corneal ulceration/keratomalacia)
Stromal defects occur in the late stage due to colliquative necrosis and take several forms.
Small ulcers (1-3 mm) occur peripherally in inferior of nasal aspects, setting in xerotic cornea.;
they are characteristically circular, with steep margins and are sharply demarcated. (round or oval ‘punched out’ defect
Large ulcers and areas of necrosis may extend centrally or involve the entire cornea.
Keratomalacia (Sterile corneal melting by liquefactive necrosis) - characterized by rapidly progressive localized melt involving entire corneal thickness.
Begins as opaque grey lesions or in severe VAD as sloughing necrotic stroma resulting in a large ulcer or descemetocele, which may result in perforation which heals as dense, white, peripheral adherent leukoma.
Secondary infection might occur.
If appropriate therapy is instituted immediately, stromal defects involving less than one-third of corneal surface (X3A) usually heal with scarring, leaving some useful vision. However, larger stromal defects (X3B) commonly result in blindness.
 |
| Figure 4. Corneal ulceration (X3a) without secondary infection |
 |
| Figure 5. Corneal ulceration (X3a ) with secondary infection |
 |
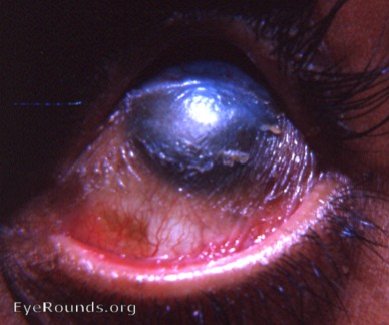
| Figure 6. Keratomalacia |
6. XS (corneal scars).
Healing of stromal defects results in corneal scars of different densities (nebula, macula or leukoma) and sizes which may or may not cover
the pupillary area. A detailed history is required to ascertain the cause of corneal opacity.
staphyloma, descemetocele or phthisis bubli (due to perforation with intraocular content extrusion)
 |
| Figure 7. Corneal scarring |
7. XFC (Xerophthalmic fundus).
It is characterized by typical seed-like, raised, whitish lesions scattered uniformly over the part of the fundus at the level of optic disc.
Small white retinal lesions accompanied by constriction of visual fields
Retinopathy, characterized by yellowish peripheral dots in advanced cases and is associated with decreased electroretinogram amplitude.
Response to Vit A – disappears in 2 to 4 months of therapy
Treatment
Keratomalacia is an indicator of very severe vitamin A deficiency and should be treated as a medical emergency due to the risk of death, particularly in infants.
It includes local ocular therapy, vitamin A therapy and treatment of underlying general disease.
1. Local ocular therapy.
For conjunctival xerosis- Intense lubrication.
Artificial tears (0.7 percent hydroxypropyl methyl cellulose or 0.3 percent hypromellose) should be instilled every 3-4 hours.
Topical retinoic acid - may promote healing but is not sufficient without systemic supplements.
In the stage of keratomalacia, full-fledged treatment of bacterial corneal ulcer should be instituted.
Corneal perforation is addressed surgically as necessary – Therapeutic corneal grafting to restore tectonic integrity of eye
Optical iridectomy or optical penetrating keratoplasty for corneal scar
2. Vitamin A therapy.
Treatment schedules apply to all stages of active xerophthalmia viz. XN, X1A, X1B, X2,X3A and X3B.
Oral administration is the recommended method of treatment.
However, in the presence of repeated vomiting and severe diarrhoea, intramuscular injections of water-miscible preparation should be preferred.
The WHO recommended schedule is as given below:
i. All patients above the age of 1 year (except women of reproductive age):
200,000 IU of vitamin A orally or - (66 mg retinyl acetate or 110 mg retinyl palmitate orally)
100,000 IU by intramuscular injection- (55 mg water miscible retinyl palmitate I.M)
Schedule : timing given immediately on diagnosis and repeated the following day and 4 weeks later.
ii. Children under the age of 1 year and children of any age who weigh less than 8 kg
should be treated with half the doses for patients of more than 1 year of age.
iii. Women of reproductive age, pregnant or not:
Those having night blindness (XN), conjunctival xerosis (X1A) and Bitot’s spots (X1B) should be treated with –
a daily dose of 10,000 IV of vitamin A orally (55 mg retinyl palmitate-1 sugar coated tablet) for 2 weeks.
For corneal xerophthalmia, administration of Full dosage schedule (described for patients above 1 year of age) is recommended.
3. Treatment of underlying conditions
such as PEM and other nutritional disorders, diarrhoea, dehydration and electrolyte imbalance,
infections and parasitic conditions should be considered simultaneously.
Multivitamin supplements and dietary sources of vitamin A ( fish, fish liver oil, egg yolk, dairy products, green leafy vegetables, red palm oil, red-yellow-orange color fruits-papaya mango) are also administered.
Prophylaxis against xerophthalmia
The three major known intervention strategies for the prevention and control of vitamin A deficiency are:
1. Short-term approach.
It comprises periodic administration of vitamin A supplements.
WHO recommended, universal distribution schedule of vitamin A for prevention is as follows:
Infants 6-12 months old and any older children who weigh less than 8 kg.
100,000 IV orally every 3-6 months.
Children over 1 year and under 6 years of age.
200,000 IV orally every 6 months.
Lactating mothers.
20,000 IV orally once at delivery or during the next 2 months.
This will raise the concentration of vitamin A in the breast milk and therefore, help to protect the breastfed infant.
Infants less than 6 months old, not being breastfed.
50,000 IV orally should be given before they attain the age of 6 Months.
A revised schedule of vitamin A supplements being followed in India since August 1992,
under the programme named as ‘Child Survival and Safe Motherhood (CSSM)' is as follows:
• First dose (1 lakh I.V.)-at 9 months of age along With measles vaccine.
• Second dose (2 lakh I.V.)-at 18 months of age along with booster dose of DPT/OPV.
• Third dose (2 lakh I.V.)-at 2 years of age.
2. Medium-term approach.
It includes food fortification with vitamin A.
3. Long-term approach.
It implies promotion of adequate intake of vitamin A rich foods such as green leafy vegetables, papaya
and drum- sticks. Nutritional health education should be included in the curriculum of school children.


Night blindness is also k/as –Chicken eyes [since chickens lack rods & are nightblind]
ReplyDelete